The Root of the Problem
Over the past few months, I’ve been undergoing a series of extensive and thorough medical tests to get to the bottom of some physical issues I’ve been struggling with for years. Since well before these tests began, I’ve intuitively known two things to be true: something is inside me isn’t right but that whatever it is, it is treatable.
And yet, all my interactions with the American medical system thus far have led me to dead ends. Despite my history of extended international travel, few tests were run, with doctors dismissing my hunches because by most metrics, I’m a functioning individual. Instead, they assumed inconclusive diagnoses like IBS, lupus, stress, age. The solution was to relax! Drink more water! Eat more fiber! One doctor even suggested an antidepressant to help with gut issues, to which I smirked, raised an eyebrow, and resisted the urge to hand over a draft of my book along with my absurd $100 copay.
In September, after five years of this song and dance, the right professionals appeared at the right time. Instead of looking at each one of my issues in a vacuum, as if each symptom existed independently from the rest, my team analyzed my lab results and lifestyle from the perspective of an interconnected organism.
A saliva test, for example, indicated high cortisol (stress) levels but nonexistent estrogen and progesterone (sex hormone) levels. Looked at independently, the answer is hormone therapy that lowers cortisol and raises estrogen and progesterone. Simple, right?
Nope. A urine analysis revealed nearly nonexistent levels of metabolized cortisol, and a blood test showed signs of kidney dysfunction. Therefore, it’s not that my body produces too much cortisol, it’s that it can’t process it, which is a totally different problem that would not be fixed by lowering cortisol through drugs.
Still, this wasn’t the root of my complicaitons. My poor cortisol production was a symptom of a greater issue we discovered: a raging bacterial infection and parasitic presence, likely picked up while I was traipsing around the globe back in 2016. The constant stress of the infection increases cortisol production (and therefore lowers sex hormones because evolutionarily, it was unadvisable for our ancestors to focus on baby-making during stressors like famine or tribal war.) But because my gut is renting out space to unwelcome squatters, it’s not absorbing nutrients or electrolytes. Thus, I’m dehydrated no matter what I drink, which explains the kidney dysfunction, and the kidney dysfunction leads us right back to….poor cortisol processing! Hallelujah! Answers!
Why am I telling you this?
Two reasons. First, my gut bug story is a reminder to follow your intuition when it comes to your health. Half a dozen doctors dismissed my complaints, for years. I get it. They’re trained to look for extremes and to fit people into boxes of symptoms because that’s how we bill insurance companies. But the only person who knows you, is you. If you’re not a hypochondriac and you think something is off, follow that thread. Either you don’t find anything and you can breathe easy, or you turn out to be right.
Second, in going through this process, I was struck by how a whole-body approach to physical health is so similar to successful treatment of mental health. In both cases, few professionals actually look at comprehensive systems. An internist analyzes the gut and an endocrinologist analyzes the hormones, but at no point does either specialist talk to the other. The same is true for our approach to mental health. If you meet the criteria for depression, a psychiatrist gives you a diagnosis and a prescription slip. If you’re lucky, you work with someone who lets you talk a little bit about your wounds and your stressors for forty-five minutes, once a month.
While a series of lab tests were able to diagnose my root physical issues (the rent’s about to skyrocket, gut bugs), it’s rare to find people who are willing to dig around for root issues in their psyche. This work requires radical acceptance, ferocious commitment, and an unrelenting belief that it is possible to heal. It will ask someone to face their deepest shame, make extreme changes to their life, and to prioritize this work above all else. It requires financial commitment. It often gets worse before it gets better. It is hard. But it is also how we heal, how we build the strength to support a beautiful life.
I will be spending the next six months on a strict diet & supplementation schedule to evict the unwanted tenants living in my belly. What if you also spent the next six months committed to your physical and/or mental health? What if you went all in and committed to addressing the issues you know, intuitively, are bubbling inside your mind or body? What if you trusted that the work would pay off? What might your new life be like?

Need a little giggle? Order one of my Fuckit Buckets™.
Look, we know that life is a special sort of disaster right now. Your closet is your office, the kids are still at home, and still your mother-law is calling you fat again. Let this little charm be a reminder that sometimes you have to chuck it in the Fuckit Bucket™ and move on!
Coming September 6, 2022
May Cause Side Effects
Brooke’s memoir is now available for preorder wherever books are sold.
This is a heart-rending and tender memoir that will start conversations we urgently need to have. It’s moving and important.
Johann Hari, author of New York Times bestseller Chasing the Scream and international bestseller Lost Connections: Uncovering the Real Causes of Depression—and the Unexpected Solutions
More articles from the blog
see all articles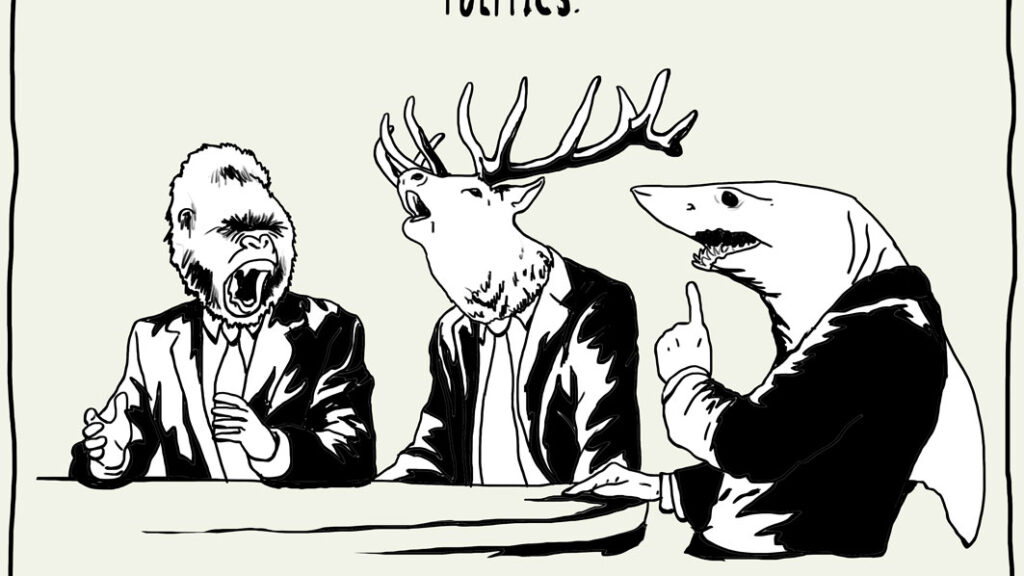
October 28, 2022


















